ORGAN DONATION LEADING PRACTICE
Current leading practice in organ donation is a whole-hospital system to manage the deceased organ donation process. This system has been implemented within hospitals worldwide and has effectively increased the rate of deceased organ donations.
Leading practice in organ donation refers to the best known way to complete each action in each step of the organ donation process; from identifying a potential deceased donor to achieving a successful, life-saving organ transplant.
An important aspect of current leading practice in organ donation is the requirement that each hospital has a team of qualified and experienced medical professionals dedicated to the task of identifying potential donors throughout the entire hospital, and ensuring families have the support and information they need to make the difficult but life-saving decision to donate their loved one’s organs.
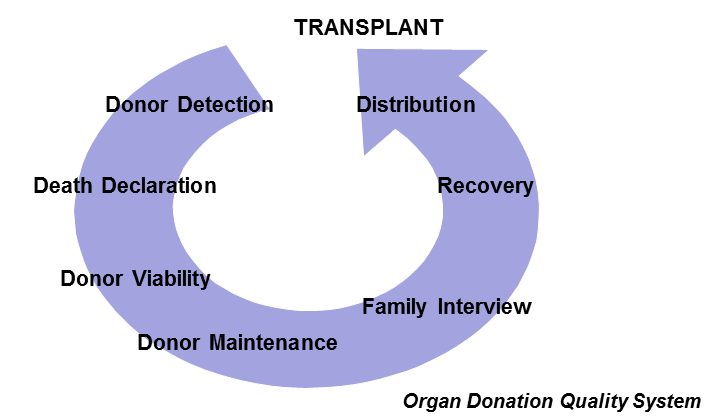
The deceased organ donation process takes place within the hospitals. It starts with the identification of patients who are potential deceased donors and finishes with the transplant. The deceased organ donation process involves a range of complex healthcare activities and communication from within and between hospitals and across local, regional and national environments. It is therefore essential to establish a systematic process within the national authority responsible for organ donation in order to optimise, track, manage and measure its development and effectiveness.
The Sydney Local Health District has developed the Organ Donation for Transplantation Plan 2014-2017 which outlines how the Royal Prince Alfred Hospital plans to implement leading practice:
> > Read extract showing implementation plan. This is an example of the Leading Practice Process in Practice from Royal Prince Alfred in Sydney that was launched in August 2014.
DECEASED ORGAN DONATION PROCESS
Leading practice in organ donation requires effective delivery of all actions in each step of the deceased organ donation process to achieve the optimal outcome. This model has significantly and rapidly increased the rate of deceased organ donations in hospitals worldwide.
1. DONOR DETECTION
Donor detection is the most important step of the deceased organ donation process. In general terms, any patient who dies in a hospital could become a possible donor (organ and/or tissue donor). This means that all key areas such as Accident and Emergency, Intensive Care Unit and Wards need to be actively engaged in the organ donation process – all hospital staff need to be engaged for this step of the process. Leading practice aims to identify every single possible donor at the donor detection stage by ensuring all relevant staff are actively and effectively engaged in the detection process.
From the potential donors identified, only 50 to 70% become an actual organ donor. This is why it is important to implement a proactive whole-of-hospital system for early identification and to refer all possible donors from every hospital department. All treating physicians, dedicated donation specialists and nurse staff are responsible for detecting and referring any possible donors.
2. DEATH DECLARATION
The deceased organ donors can be classified into two types according to the diagnosis of death: Brain Death or Circulatory Death.
- Brain death is the irreversible cessation of all brain activity, including the brain and brain stem. Brain death donors are those patients in whom, after suffering a severe brain injury, death is diagnosed according to specific neurological criteria, while respiratory and cardiovascular functions are maintained artificially.
- Circulatory death is the irreversible cessation of all circulatory and respiratory function. Circulatory death donors are patients in whom death is certified according to circulatory and respiratory criteria.
Leading practice requires implementation of a clear and systematic protocol for death declaration. The protocols should be known and followed by key hospital staff.
The Australian and New Zealand Intensive Care Society Statement on Death and Organ Donation provides the framework for best practice in the determination of death, aspects of end of life care in the intensive care unit, and best possible care for the patient and their family. The Statement summarises the evidence-based approach used in Australia for determination of brain death by intensive care specialists.
In Australia the determination of death and the conduct of organ and tissue donation are undertaken in accordance with defined medical standards and within legal requirements.
3. DONOR AND ORGAN VIABILITY
Donor and organ viability are the measures taken to evaluate medically suitable donors. The objective is to avoid or diminish the risk of disease transmission to the organ recipients and to ensure the functioning of the organ after the transplantation.
There are absolute medical contraindications for rejecting the donated organ for transplantation i.e: metastatic tumors and general active infections (sepsis). In these cases none of the organs can be used for transplant even though the families consent to the donation. A well-trained donation and transplantation specialist team are the key to the proper evaluation of each possible donor.
4. DONOR MAINTENANCE
After the confirmation of death, the protection and functional maintenance of the organs intended for transplant is the primary objective. Brain Death causes severe physiopathological changes in the cardiovascular and respiratory system as well as changes in the hormonal and metabolic balances. It is described that about 3.1 % of brain death donors could be lost due to problems with maintenance. Applying standardised protocols and algorithms will reduce the loss of organs and improve the functionality of the organs transplanted.
Gelb et al. (see article here) proposed the “Rule of 100” as the goal to be achieved during the donor maintenance: Systolic arterial pressure: 100mmhg; urine output >100ml/h; PaO2> 100mmHg; Haemoglobin >100g/l.
The Donation Medical Specialist is responsible for leading the donor maintenance and to implement a review process for each case in order to provide feedback and optimise the maintenance of the donor.
5. FAMILY INTERVIEW
The family conversation is a dynamic process, centred around supporting families who are experiencing acute grief, enabling them to make informed decisions about organ and tissue donation. The events that surround the death affect each member of the family emotionally and physically. A professional team dedicated to supporting the grieving family should identify and manage those individual needs.
6. ORGAN RECOVERY
The logistics and coordination of the different transplant teams starts when the donation is agreed to by the relatives of the donor. The organ recovery requires collaboration between the different hospitals and teams involved in the procedure to achieve on-time retrieval of the organs and preservation of appropriate conditions until the transplant. Two groups (abdominal and thoracic teams) are organised to perform the organ recovery; an additional team is required for tissue recovery. Tissues recovered include cornea, skin, bone and heart valve. Organ recovery should be considered an emergency procedure with priority access to the operation room. Organ and tissue recovery are sterile surgical procedures where all aseptic techniques are preserved.
7. ORGAN DISTRIBUTION
There are more people waiting for transplant than organs available, so objective, clear and transparent rules must be in place to determine the allocation and distribution of the recovered organs. The organ allocation should be guided by clinical criteria and ethical norms. The allocation rules should be equitable and externally justified. When the organs are successfully allocated a logistics team will transport and distribute the organs to the selected recipient.
8. TRANSPLANT
The transplant is a surgical procedure that replaces a damaged organ by another organ with same characteristics. A transplant cannot be performed without an organ donor.